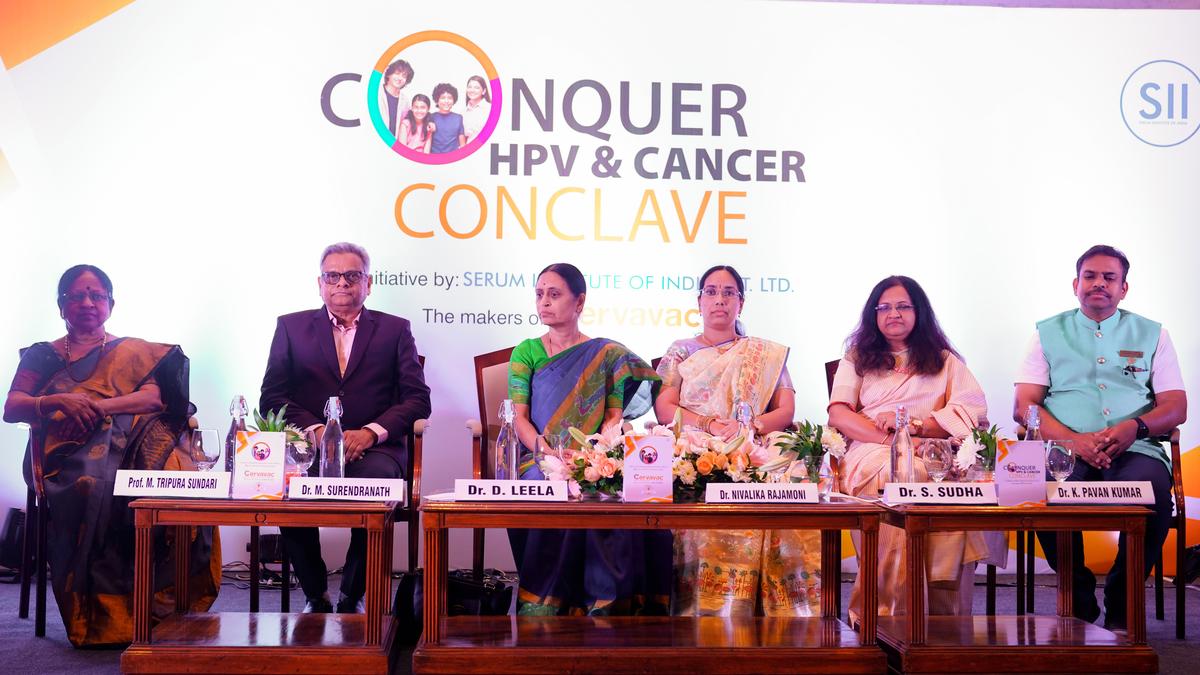
(left to right) Prof. M. Tripura Sundari, Dr. M. Surendranath, Dr. D. Leela, Dr. Nivalika Rajamoni, Dr. S. Sudha and Dr. K. Pavan Kumar at Conquer HPV and Cancer Conclave in Hyderabad on Thursday.
For years, the human papillomavirus (HPV) vaccine has been closely associated with preventing cervical cancer in women. However, doctors are now pushing for a more inclusive approach, urging that boys too be vaccinated to curb transmission and protect against several other cancers linked to the virus.
At the Conquer HPV and Cancer Conclave, an initiative by the Serum Institute of India in Hyderabad on Thursday, doctors underscored the need to reframe HPV as a public health concern rather than solely a women’s health issue.
“Why boys? Because they are the carriers. HPV is primarily transmitted through sexual contact. In both Indian and Western statistics, about one in three boys are found to have the virus by the age of 15. While it may not cause immediate symptoms or health issues in boys, it is often passed on to girls, increasing their risk of cervical cancer,” said Dr. M. Surendranath, HoD, Paediatrics, DNB Faculty, Vijay Marie Hospital, Hyderabad.
He pointed out that HPV is not limited to cervical cancer. “It can also lead to penile cancer, anal cancer, and oropharyngeal (throat) cancer in men. Moreover, HPV types 6 and 11 cause genital warts, psychologically distressing, though not cancerous. Australia’s decision to vaccinate boys under its national immunisation programme has significantly brought down cases of genital warts,” he said.
Silent virus, late consequences
One reason for the lack of awareness, doctors say, is that HPV doesn’t show symptoms early on. “It is unlike other viral infections where you get a fever or rash. In the case of HPV, most people don’t even realise they’ve been infected. It can remain dormant in the body for decades and only manifest as cancer years later,” said Dr. D. Leela, consultant gynaecologist, St. Theresa’s Hospital and Asvins Hospital, Hyderabad.
Screening and prevention: Not just vaccines
While vaccination is a crucial step in prevention, doctors highlighted the importance of screening, especially for women aged 30 and above.
“There are three levels of screening. The government-recommended method is VIA (Visual Inspection with Acetic Acid), where simple vinegar is applied to the cervix to check for abnormalities. Then there is the more familiar Pap smear or cytology. And finally, the most sensitive but costly option is the HPV DNA test, which detects the presence of the virus directly,” the doctor added.
Vaccine targets and coverage
The most commonly used HPV vaccines in India are quadrivalent, targeting types 6, 11, 16, and 18. While 6 and 11 are responsible for genital warts, 16 and 18 account for over 80% of cervical cancer cases. “As far as genital warts go, they are relatively uncommon in India compared to Western countries. In our clinical experience, they account for about 5 to 10% of cases in gynaecological practice. Many of these patients go to dermatologists instead,” said Dr Surendranath.
Published – July 25, 2025 12:37 am IST